Medical Student Stuff
Pediatric Rotation — Over
About the format of this post, it’s sort of odd. Perhaps, one day, I’ll go back and editorialize this entry. For now, I’ll just stick with the facts my version of reality. Depending on the program, the Pediatric grade structure will vary. Most will have the same elements, clinical evaluations, activities you have to do, shelf exam or in-house exam. The shelf is a national, rotation dependent test, and an exam with standardized convoluted questions — because if they just asked you a straight forward question, and you answered correctly, where would the fun in that be? All of those elements, will be lumped and weighted together to form your grade: Honors, High Pass, Pass, and perhaps Low Pass. At my program, regardless of being on an away rotation, our grade is built mostly by evaluations from attending or resident physicians. In any event, this post will include some details about the structure of my Pediatric Rotation.
Location – a community hospital operated by Awesome General Hospital
Time – 6 weeks total, average work with 50 hrs (including didactics)
- 2 weeks on ED Pediatrics, mostly traige type of thinking; one on-call shift
- 1 week on Special Care Nursery, pre-round, round, write progress notes
- 3 weeks on Pediatric Inpatient Wards, gather vitals, round, check on patients throughout the day to assess the patient and how the plan is going, make lots of phone calls (talk to radiology to get help with a X-ray, make an appointment for the patient for follow-up care, talk to social workers; one on-call shift
- Weekly, half-day, ambulatory Pediatrics,
- One home visit to someone physically and/or cognitively disparity
Structure
The structure was dependent upon service and the whim of whoever attending I’m who’s on service.
ED Pediatric – this was my first excursion into Pediatrics, my patient loaded included whoever came in; however this service required very little management from my part as just about everything was algorithm based.
Types of cases: I saw the bread and butter stuff you expect to see: worried parents rushing in their newborns because of a fever (ending up with a urine analysis, blood work, and a lumbar puncture), concussions (I was usually given the task of telling the parents why we weren’t getting a CT), asthma, teenagers impaling themselves with objects (the oddest being a carabiner), sniffles, rashes, and one murmur that I got to diagnose and refer to cardiology for follow-up at Awesome General Hospital.
Structure: there were certainly lulls with nothing to do followed by bouncing around to room to room to see patients. Before seeing the patient, if I was lucky, I’d get the nurse’s “in-take note” (the reason why the the patient came, vitals, and a brief history when they were triaged). I’d walk into the room, introduce myself and role, get a quick targeted (but full) history of present illness and past medical history, do a review of systems, perform a targeted physical, then summarize an initial plan with the parents. The next step was to present the relevant parts of the case to my attending (there were no residents on this service, so medical students were the ‘residents’), and then I’d go over the plan that I thought of (aka winged) — the most important part of this conversation with the attending was to be efficient, they usually wanted a really quick explanation. Sometimes, we’d go back in the room together, the physician would do their own exam, repeating whatever they thought was worthwhile, and they’d either agree or modify my plan.
Summary: the cases were interesting, and I gained a skill at attending telepathy a.k.a. taking a guess at how much to summarize a case.
Special Care Nursery – my second service on this rotation. I was responsible for one to two patients per day.
Types of cases: as a newborn, you’re either put into a nursery if you’re healthy, a NICU if you’re really sick, or a special care nursery if you’re somewhere in between. As such, I saw and managed patients with prematurity complications, jaundice, failure to thrive, observation for murmurs and breathing difficulties, and neonatal abstinence syndrome (NAS). I took a special interest in the NAS babies, I had worked with mothers who were exposed to narcotics while pregnant during my Ob/Gyn rotation (some mothers were even from my home hospital in Boston, World’s Best Safety Net Hospital). So, it was a nice longitudinal experience. My previous rotation was Ob/Gyn, I learned a lot, but nothing about babies (or anything about children for that matter). However, I have a pretty good handle over pregnancy and woman’s health now, it helped that I’ve already been on the giving the baby away side of a birth. Now, on the receiving end of deliveries, performing neonatal resuscitations, the experience felt more complete.
Structure: again, there were no residents on this service, so you expected to perform a lot without much guidance. I’d pre-round on the babies, this essentially meant just copying down what happened over night in their paper chart (yes, I said paper). Then, I’d have about 15-20 minutes to get my thoughts together (aka scourer UptoDate and PubMed), and present the patient to the attending. At the end, I’d make an assessment and plan, sometimes they bought it sometimes they didn’t. After that, we’d round on the patient: check fontanelles, lungs, breathing, red reflex, check their oral cavity, and end with checking their hips for dysplasia. The remainder of my day was spent writing progress notes, most of that was rattling off a differential and justifying my final diagnosis. The day ended with the attending reading my progress note, making edits, and including my note into theirs — the most glorious moment was when an attending would just say, after signing off, “Just put your note into the chart”.
Summary: in a strange way, I enjoyed the neurotic level you have to go to manage special care unit babies. Not being satisfied with the patient monitoring my away rotations EMR had, I developed an excel sheet to finish better follow patients and write notes; I’m ashamed to say it brought out the “type A” in me.
Wards: my last service on Pediatrics, and the only part with residents; and arguably, it was the best way to end. I was responsible for 2 to 3 patients a day, depending on what was going on.
Types of cases: reactive airway disease, asthma, a bunch of pneumonia, croup, jaundice, liver problems, accidental (including some outrageous lead poisoning) or intentional poisonings, smoke inhalation after the patient’s family member tried to kill said patient, syncope, kids with seizures, and a spike in infants with viral meningitis. These were considered to be “bread and butter” cases to learn how to manage. If I had been at my home institution, or just back in my city, I’d probably see a lot of specialty cases and miss a lot of the “bread and butter”. That’s been the experience for some of my classmates who stayed in the medical capitol.
Structure: the name of the game is “family-centered-rounds“. The goal of family centered rounds, at least in theory, is to include the family into rounds. How family centered rounds play out, as I hear from residents, just depends on where you’re at and who s leading your team. In general, you present your patients in the room with the family, ask a few follow up questions, you explain the latest data to assess their child’s health, do a physical, and then tell the parents (or the patient only, if old enough) your assessment and plan for the situation. You leave the room, slip back into doctor lingo, and a period of critiques (positive and/or negative) and education starts (a.k.a. attending pimping). The rest of the day is spent making that plan you talked about come into fruition: leg work, working with the nurses, office stuff, and looking up a lot of things. Your patients on the floor who were admitted over night will need a full history of present illness note, so they can be properly admitted onto the floor. Your patients who you’re continuing to follow, or you’re covering, will usually only need a progress note. The only reason why I bring those notes up is that it’s a hell of a lot more work to finish putting together things for an admission than a progress note. Lastly, since the flow of the day was purely dependent on the whims of the attending physician, everything I said could be changed in any way they see fit — my biggest lesson, figure out what they want before you spin your wheels.
Summary: This rotation was sort of awesome because I learned how to better management patients and do doctor stuff. The difficult part about the this rotation however was differential diagnosis, i.e. the obscure stuff you didn’t learn about during the first two year of medical schools — heck, at best pediatric conditions and managements are foot-notes during the first two-years of medical school. Also, the intern and residents really improved my experience on the floor.
House visit: this was a one-time visit, we go in pairs (two medical students), and only a few medical schools in my city participate. You make one home visit to visit the family and patient as they deal with physical and/or intellectual disabilities — in my patient’s case, they had disparities in both. For my home visit, my patient was a teen with cerebral palsy (and bulbar palsy), and he required a computer to communicate with us. We spoke with the family about how this situation came to be, the affect their other children, how it affected their relationship as a married couple, and how they’re dealing with the finances. Last but not least, we got to know our patient.
Shelf Exam
Took the shelf today, next week I’ll know how I did. The exam is administered around the same time, in an official process, for many medical schools. Unfortunately, at least in our school and some others, our tests froze today on multiple occasions. This added about 30-40 minutes to our sitting time, while somehow syphoning off our test-time. In the end result, from our post test grumblings, was a reduction in time that left most of us with only a few minutes to 30 seconds on the last question. Fortunately, because I was skeptical about if the clock was running while my questions failed to load, I was too paranoid to take a bathroom break and ended up having a couple of minutes. For this exam, I used Pre-Test Pediatrics, Blue-Prints, some BRS, and a few slide decks gifted to me from others.
What’s Next?
Psychiatry at the VA! I’ve recently filled out a mountain of paperwork, I received an email today that I’m ready to go. I start this, after the weekend, this coming Monday.
That’s it for now, have a great weekend!
Probing People and Updates
So, I just had a test on how to use all of this stuff:

- one reflex hammer
- one 128 Hz C note tuning fork
- one 512 Hz C note tuning fork
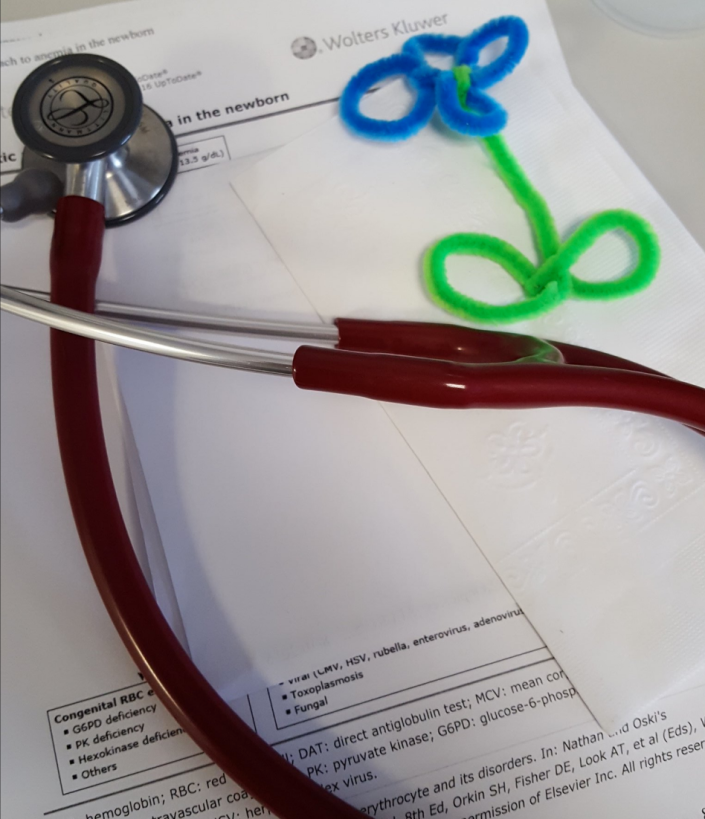
- one Littmann Cardiology III stethoscope
- in the bag, there’s an ophthalmoscope and an otoscope that also check the nose should you change speculums
- in reality, with the exception of the stethoscope and the reflex hammer, and perhaps a tuning fork I expect most things to be found in patient rooms so I don’t haul this stuff around
Next year, or rather towards the end of my 3rd year as a medical student, I’ll take STEP 2 of my board certification. You’re expected to know how to use the stuff in the above picture and show off your clinical prowess in other ways. My school year ends in less than 3 month! It’s hard to believe that in less than 3 months I’ll be heading towards the 3/4th point of finishing medical school — I pick my 3rd year rotations (including elective rotations) in a few weeks. It seemed to have taken so long to have gotten here, and yet it seems to be flying by a lot quicker than expected.
Anyways, with all that aside, to prepare for the 3rd year we performed a 250-point physical on a standardized patient. Over winter break I had illustrious dreams of practicing the physical, way before the deadline I contemplated, perfecting my craft. This didn’t happen. But, at least temporarily, I did lose the bags under my eyes. This was a small life-cycle victory for myself. I was able to practice, just the day before the exam, once with a classmate and multiple times with my partner — it’s a time consuming process, I still owe her dinners till this day to make up for it. Mike, my standardized patient was also a great person to examine. Likely well into his mid to late 50’s, Mike was well built (likely more muscular than I, not that I’m all that impressive of a norm) and a talkative native of Boston; accent included. I invited him to talk the whole time, though there are times where quiet is necessary, I find examining patients while they talk to be a lot more natural than probing them and reaching into their nether regions in stone-cold silence. Mike told me he’s into sports, so we spoke about sports while I give him a physical from head to toe (literally). The most difficult part of the exam was that I actually don’t watch or care about sports, with the exception of the Olympics (oddly enough, I haven’t missed any for the last 12 years). I grew up in a sports loving family, if you didn’t play sports you were considered weird, I played: baseball, basketball, football, and even golf. I fell out of love with watching sports a long time ago, just quitting cold turkey. But, I know the buzz word things to talk about in sports conversation. Though, somehow, sometime later we got into a conversation about our mutual love for the smell of Christmas trees. Yes, specifically the smell, how else to test cranial nerve I?
After the exam, while emphasizing my lack of knowledge, I told him ‘off the record’ that one of his arteries was bounding more than I would like. I asked him if anyone had ever told him something like that before, he said in fact they had. The finding could have been benign, but after we spoke he agreed it’d be best if he’d go ahead and check it out. He asked for a mole check, did the basic ABCDE, and seemed like just a normal mole — apparently, others he asked were also in agreement. Besides some typical features found with aging, he was perfectly healthy except for a slightly non-malignant high blood pressure that he was concerned about because he’s historically 120/80. He cared about his health, I could appreciate that. We spoke more about that, I asked him more about his substance use, in this case coffee that he remembered drinking (2-3 cups a day). We agreed that at his next visit he’d skip the coffee and then see if he’s back to normal, then take things from their with his doctor.
It’s funny, when I started the exam, I had heard that this is just a dry-run: you just have to speed through the 250-point checklist like they’re a car at Jiffy-Lube. Instead, I was met by a man, a patient who actually was both teaching me and hoping to get a medical benefit from the examination. And for me, that felt a lot more natural: me trying to give him a benefit. I’ll try to remember that as I practice my skills with patients in the coming days.
Today, we just finished our Rheumatology unit, I enjoyed it more than I expected. It was challenging, but a fair unit. During that unit, I went back to refresh myself on medical microbiology (Sketchy Medical, First Aid and UWorld questions). Some days I’m scheduled at a local community health center, we’re farmed out to a lot of places but I was fortunate to pull one that’s easy to get to. We’re now required to have one clinic day where we see patients, where we perform a battery of histories and physical examinations. I’m looking forward to returning to clinic, it does take some time out of my study schedule but it helps to remind me of why I want to do this in the first place. Though, I prefer being in a more intensive setting, so I’m also schedule to hop onto cardiology wards this coming week the day after the health center. As such, I decided to start reviewing cardiology again in my board studying schedule this weekend. Given that I’ve rounded with this attending before, my PI (he’s an Atrial Fibrillation (AF) specialist), I’ll review the basics before I show up: drugs (their indications and side effects in regards to), certain high yield risk analysis scores like the CHA2DS2-VASc Score for Atrial Fibrillation Stroke Risk, ECGs, murmurs, etc. With the cardiology team, it’s quite large, and there’s a lot that needs to get done so I don’t expect to be called on or present. But, I feel I should at least put in the effort to understand the answer that my seniors are being politely pimped about; it does seem at least common courtesy. Knowing stuff helps me pretend I know what’s going on, it’s an important strategy.
Tuesday, we start Renal Medicine. Should be a tough course, though it’s pretty much just a down hill slide from here as long as I keep on schedule. Thus, I’m looking forward to it and the patients and experiences I’ll incidentally meet along the way.
My Podcast Interview With Accepted.com – Medical School Admissions
Hello everyone,
A few week ago, I think a day or two before some exam, I sat down to do a podcast interview Accepted.com.
We spoke for about 45 minutes about medical school and my own medical school admissions experience.
So, if you ever wanted to hear me blabber on about medical school, here’s your chance:

Exam Went Great — And Background Maintenance, Forgive the Mess!
Hello,
So, the last time I left off on this blog I was having a happy-go-lucky the night before my Endocrinology exam. Great news, my chicken to egg ratio estimation was pretty spot on, the exam went remarkably well — in fact, it’s was my personal best since I started medical school. Academically, a lot of things happened just at the right time to make it happen, and a lot of that is because I have a solid and dependable study partner. A lot of us live off campus, so we have many off campus study habitats. One day, we expanded the study group, did practice questions, then discussed every option either right or wrong. It doesn’t take that long to do this by yourself, because you only have your internal dialogue to contest with on topics. Add in another person, two type-A medical students, the time takes longer but you each individual gets more out of it; probably because you can’t just appease yourself any longer. Add a few more people, toss in contrasting personality types, and well you have an all day affair. But, it was well worth every minute. I think having to explain my ideas or theories of why an answer is right in front of my peers, friends with very low tolerance for BS or fluff answers, was a great measure of my understanding. Also, while working on problems I’m not so shy to just say, “I don’t get X, can you explain it to me?”, when I see people who’ve mastered a certain topic more than I — it helps that I know down to earth people who’ll easily say the same thing to me. Anyways, I’m an advocate of studying independently combined with study groups, and I mean really studying in groups not just “parallel play” studying.
Blog Maintenance
I’m on vacation for a few more days, on Monday we start Dermatology (rash city). I have a few random life things to do, apply for a state ID, register for boards, and start scouting for a new place to live for summer before clerkship starts/in between boards. But, for now, I’m going for a small victory of organizing my blog a little. I’ve gotten a few fist-shaking emails asking to make my entries easier to find and search. I’m not a web administrator, and it’s just a blog, but I’ll try to tidy things up on the backend a bit. I figured now’s a decent time, as most premeds who still visit my blog have already applied to medical school this cycle and my blog doing strange things wouldn’t adversely effect them. One of the biggest shifts will be the destruction of all the categories. My blog started just as a post to document my process through medical school, and I haphazardly added categories as the things I spoke about grew. So, I’ll be fixing the categories, with a more limited filing option to make things more logical. Also, I’ll go back and see what I can do about tags to make things easier to search. I appreciate your emails, and the fact that you bother to read and want more out of this odd social experiment that is my blog. I have about +160 articles here to work on, so give me a little time and things will hopefully be smoother!
Medical Endocrinology Exam in the AM — And I’m Okay With It!
Hello,
As the title alludes to, I have an exam in the morning to start my day at 8 AM. Followed by that, I think I have a free spat of time in the afternoon to hang out with friends (since I’m away from home, all of my friends in Boston are now medical students or doctors now). Though, around 3 PM, I’ll do my service learning experience — I’ll be in the anatomy lab with high school students and talking about lungs, should be fun. A lot of medical students, at least the one I go to, pursue a lot of special interests on the side. It’s common for medical students, I assume across the country, to volunteer their time outside of their coursework. I assume, like me, a lot of people find having an experience outside of syllabi to be mentally therapeutic. I’ll get home at around 6 PM, maybe eat dinner and watch rewatch Scrubs, or maybe make it a date night.
The interesting thing is, all of this is happening tomorrow and the exam bothers me the list bit. I’m actually looking forward to it, mostly because I get a week’s vacation (minus clinic hours) from class. While I still have a lot to learn, I’m learning to really value what’s important in medical school: being healthy. So, though I’m really looking forward to the vacation I’ve also tried to follow the stride of some of my other classmates’, and strive for a better work-life balance. My days of taking vacations like this are numbered, so it’s important to learn how to just enjoy what I’m doing instead of just waiting till the next extended vacation to get affairs in order.
After weathering the storm of an over committed first year, I’ve (and I hope others) found second year to be both healthy challenges and at the same time an epically better experience than the first year. I’ve grown a lot closer to my classmates, and think of some of them as family (cousins perhaps), and when working together everyone is extremely helpful and bright. This year, I participated in a program where I shadowed charge nurses at one an “away” hospital. This was a great experience. I tossed on my short white coat, tied my stethoscope into a loose pretzel knot and stuffed it into the white coat pockets. Jammed my pocket Bates into the other, I thought about smuggling a sandwich but that seemed obsessive. I clipped on my name tag and called a Lyft to give me a ride to the hospital, as it was quite a trip with public transportation — and really, time is money. I arrived, and after wandering around the maze of the new hospital, I found my station and charge nurse I’d be shadowing for the day — okay, actually what really happened was I saw one of those robots that travel around the hospital, followed that a bit, then ran into a new rotation 3rd year who was also wandering around, then I found the cardio nurses station.
In any event, the nurses were all great people and taught me a lot of things, I got to see the hard work nurses put in, and working and eating together we all had a lot of laughs together. The hospital EHR was not exactly the same as our, but it was similar enough to jump on the computer to learn more about the patients we were rounding on. We were keeping close watch on one patient with Clostridium difficile, complicated by heart failure, arrhythmias, and many years of smoking cigarettes. I gave listened to his breath sounds with the charge nurse — he still heard crackling sounds in both his lungs, typically a sign of a fluid that shouldn’t be there. We then gave him his nebulizer treatment. I stretched out the hunter green elastic strap of the nebulizer mask, tossed in the dose the nurse gave me, and turned on the air. I’ve seen this done many times, but usually it was having someone do it to me. At that time, and though I have a long haul ahead of me, I realized more than ever that I’ve truly happy with my decision to attend medical school including all of the bumps that come along with it. I remembered that one of the big reasons why I wanted to be here is because I wanted to feel like I was “paying it forward” for all the times physicians and nurses helped me growing up. And, I remembered that I never predicted I’d actually be in this position to fulfill my wish as a kid to validate myself by paying it forward. So, despite there being a huge looming exam in the morning, and the mountains of debt, I’m sort of totally okay with it.
Wish me luck!
Half Way Through MS2 – Studying for Boards
Hello,
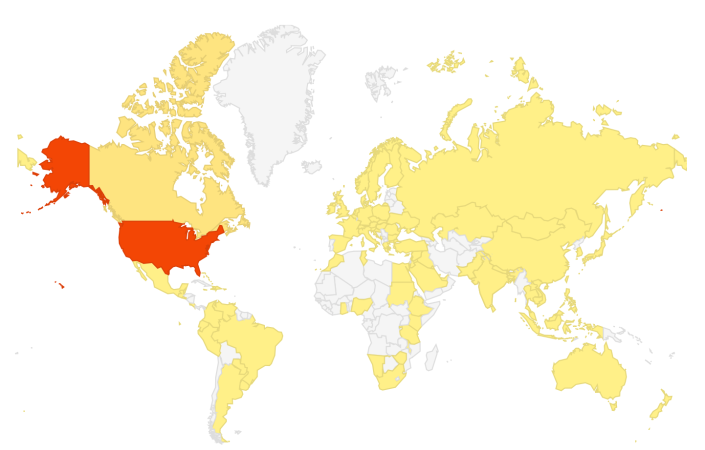
From Boston, happy autumn! Here’s a picture near my house.
Around this time of the year, squirrels should have already built their nests, and premeds are getting interviewed at medical schools. Third year medical students no longer exist, and fourth year medical students are taking care of their residency process. For me, I’ve just past the midway point of my second year of medical school and board examination. A few weeks ago, I started to prepare for the boards. When people decide to prepare for the boards is up to them, each medical school gives their second year students time off before their examination to dedicate their time to it. However, due to the high stakes of your permanently recorded score, must students start preparing for it earlier — some students have started studying since last year, some started this summer, the large majority seem to wait until fall or winter to start thinking about it — it’s a personal choice when you decide to start it. For myself, I have a hard time evaluating what I do and do not know, so answering questions works for me whilst taking the same course: I do psychiatry questions during the psychiatry section of class. In essence, I’m trying to eat my cake and have it too, I’m trying to use the boards as an adjuvant to class or vice versa.
If you’re not familiar with the boards, and most notably the question style, this succinct best flow chart below explains the situation the best…
Here are the resources (besides lecture material) I use, so far:
- Goljan (high yield notes) – there’s a mix of materials, written and audio, you can choose what works for you.
- Board Review Series (BRS) – I supplement this when needed. The lecture notes will be more detailed, but BRS is best used IMHO to get the big picture.
- First Aid (notes) – I’ve started to just take notes straight into it. When I get questions wrong (any question bank), I just look up the topic in First Aid, see if it’s a fact that I never heard of or not, then I finally just annotate straight into the book.
- Sketchy Medical – this is a must have for all second year medical students. You will feel absolutely ridiculous using this in public, but your blushes are worth the pay back. I watched the videos and used the provided PDF ‘images’ as Anki (flashcards). Thankfully, they’re coming out with a Pharmacology series, I will definitely pick that up.
- UWorld (question bank)- the school strongly suggested we just stick to UWorld and some other materials they’ll update us about later, they also told explicitly told us to avoid a certain company. We were told they ask the appropriate level of third order question that we should see on our boards. I started with just doing 3 UWorld questions a day, I started only within the same subject as I was learning. Now, I do 6 in-subject and 4-5 previous subject questions. Afterwards, I just review what I got wrong and annotate that into First Aid.
- Anki – I’ve used it intermittently. It can get sort of boring to do, but it does help a lot if you just have to remember a lot of details. For myself, I’ve learned the simpler and less “busy” the card the better and faster I’ll memorize the card duo. The trick to making Anki useful is to speed up the rate it takes you to make cards. If you have a diagram, table, or image to memorize then use image occlusion. To my knowledge, and at least on my Mac, image occlusion is either missing or obscured away in the Apple compatible version. If you’re using an Apple, then you can install Wine. The Wine program will allow you to run windows programs on your Mac. If you design a two-item table in Excel (both Windows and Mac), then you can save it as a .CSV. A lot of people don’t like using Anki because it takes too much time to make cards. I remember, in my first year I’d spend hours making cards, now it only takes about 20-minutes to do the same amount of work to make them. For me, it was just important to not try to make a card for every little detail and not lose focus of the medium and big picture.
- Doctors In Training (DIT) – I just received a confirmation order, and I should be receiving it soon. I’ve heard very positive things online, especially last year when second year students were tweeting about their board results. When I get some time to sit down with it, I’ll update this blog with a review of how it worked for me.
- Pathoma – it seems like I’m the last person in my class to use this, but I just started to try it out this week.
- PubMed – often, a handful of lectures can be summed up by a short well written paper.
Anyways, that’s what I’m doing for the boards. I really don’t like adding new things into my study schedule — the more wonderful the tool the more time it usually takes to learn how to use. For this, I use First Aid as my nexus of information by taking notes into it. If I see an article on PubMed that explains it the best, then I write down a couple of words plus the PMCID so I can look it up later. So, for any source of information (especially when using multiple) I find it’s important for me to keep good track of references. I’ve even found it useful to cite First Aid pages within First Aid itself, for example at times where two concepts go together seamlessly (in my mind). If you’re in the gallows of the first year, hang tough, when you finally figure out how to juggle flaming sharks as a MS1 you’ll be able to transfer a lot of the skills over to MS2.
I use my course grade as a barometer of how well I’m balancing my position as a medical student, research, volunteering (mentoring), shadow, clinical duty, board studying, and personal life. To pass each module you need to have an average equal or greater than 72%. This year, I follow the suggested set-point given to us by our academic advisors, I try to keep my average around 85% — I’m willing to miss a few points on a written exam if it means doing the things I like. Anecdotally, I’ve heard striking a balance is key:
- I’ve heard of a minority of students going hard on board studying, but neglecting the grades, and they had to remediate courses and lose time studying for boards anyways.
- I’ve heard of a minority of students going hard on course work (nearly achieving perfect scores), not studying for the boards until the last minute, and ultimately having to retake the boards to get a score a more representative score.
- On the flip side, I’ve heard of a smaller minority who by virtue of doing nothing else but study successfully destroy the boards and the coursework, but then had to take a gap/research year to become more competitive in terms of extracurricular — this is obviously a very specific case, and really only something worth thinking about for extremely competitive specialties. Though, in the scheme of things, this is the best of the three problem situations to have.
Anyways, have a great weekend!
Finding A Lab in Medschool
Honestly, there’s no point in being around the bush, we all know that residency programs aren’t exploded with positions nor funding. So, as a consequence, medical students (masters of hoop jumping) are interested in both learning and forming a competitive residency application. There’s lots of pros to performing research, I’ll let you speculate on what they are and choose what is most important to you. Not everyone wants to do it, nor does everyone have to, but if you like research than don’t let medical school get in your way — you don’t have to be a MD/PhD or MD/MPH to conduct projects.
Know that there’s different forms of research in the medical community, and know the pros and cons. Every type of research has it’s niche problems and it’s own rewards. I have to admit that I’ve only have done bench and clinical research, so I’m limited on other types. So, I can only comment on what I learned from working on the IRB prior to medical school about the others:
Bench Research:
Likely the hardest in terms of taking successful measurements, in fact more than half of the project may be the team just sifting through superfluous or as some would say “hearing the data through the noise”. The fool-hearty go into bench research hoping for a publication, it’s best to expect to receive the baton and pass it onto the next generation. It usually takes several years to go from concept to publication, if everything lines up, so don’t expect any immediate rewards besides intellectual and networking gains. Though, if you join an established lab you may be able to stand on the shoulders of giants and gain a publication or presentation or two.
Quality Assurance/Control/Evaluation/Improvement:
Likely one of the hardest in terms of dealing with confounders and logistics, but if the research is successful you have a decent shot at seeing the ideas of the project be put into practice (or at least attempted). However, logistically, these projects may be monsters onto themselves. I can probably write an entire article of what can go horribly wrong on these projects, even if everything is done right from the researcher’s prospective, there is no reason to assume that the project will end successfully as there’s an abundance of things out of your loci of control.
Societal Research:
Confounders, confounders, confounders. There is an illusion that there’s low hanging fruit, i.e. just think of something and try it out and it’ll count as research. But, that’s pretty far from the truth. By definition, research is generalizable and has some sort of public benefit. As a consequence, it’s very difficult to actually think and perform a research project on societal issues and have it both be valid and generalizable. I know that’s a fuzzy definition, but haven’t you ever wondered why the surveys or senior thesis likely didn’t need IRB approval? Well, it’s because it wasn’t generalizable. This is not to say that receiving IRB approval means the project was/is legitimate research, honestly a lot of the time it was just a didactic exercise that certain departments tend to have — in fact, many institutions that pump out a lot of projects have an expedited process for projects that don’t necessarily fall under the category of research but still require oversight.
My gross explanation doesn’t do any of the disciplines justice. My reasoning for bringing it up was just note that you might actually like research you may not particularly like a certain niche of it.
-
Find a subject that interests you, don’t just aim for notoriety — seen a lot of bright people get disappointed by their projects despite joining an established lab/group. I have no idea what I want to specialize in, but I did know what I wanted a better understanding of cardiology — I’ve lost a grandfather and a brother who I’ve never met to cardiac problems, a grandmother to a pulmonary embolism (technically, of venous origin, a point for the lung field). Also, perhaps because I wanted to validate my time spent prior to medical school, I wanted something where I could transfer some of my previous experience (electrophysiology). If you got into medical school by working on the social determinants of health then continue that line of work if you so choose.
2. Use the internal search within your school’s site to find people you’d like to work with, follow up with some brief reading on PubMed etc. Don’t just research your PI to be Machiavellian in intent, instead find someone who legitimately interests you. Afterwards, just fire off an email, it’s much easier to get a response to talk to a physician or professor when you’re doing so as a physician candidate than compared to undergraduate years.
3. Meet with prospective PI, test for chemistry and expectations — it’s important that you not only are at their mercy, but you also should let them know your expectations. Do you want to be part of a well oiled machine, or do you want to be one of the people who develop the well oiled machine. For my PI, I eventually exchanged a verbal check-list of things I expected to learn: how to read ECG (with cardiologist input), patient exposure, and to be involved in the planning and execution of projects. Likewise, my PI gave me their check-list of things they expected from me. It’s better to custom right your own ‘wedding vows’ than accept a stock contract. Lastly, we have a very transparent understanding that I expect financial compensation, reciprocally I should make sure I work hard enough to deserve compensation. As an undergrad it’s important to learn how to bite the bullet and earn your keep, as a graduate student it’s important to know your value and feel appreciated.
4. Find funding – prior to medical school I had no problem putting in the extra time without compensation. Funding can come in multiple forms, financial, relationships, (team building and mentoring), and entry level experience. At some point, if you’re good at something I believe you should aim to get funded. A fed and housed graduate student is a happy graduate student. Funding can be tricky, but I promise you if you knew how fight for funding as an undergrad (and/or postgrad) the tricks of the trade are more or less the same: keepings your ears/eyes open and applying for a lot of fundings and getting rejected. I applied for several sources, I started off with the largest funding sources then whittled my way down to the more modest ones. Don’t be afraid to bite off more than you can chew on grant applications, at worst you just won’t get them: I tried and failed on big name grants only to get a NIH/American Heart Association one. If you’ve gotten into medical school, being rejected shouldn’t be a new feeling, so don’t mind the endless rejections on funding. It has been a lot of work, but I’ve raised a significant amount of discretionary spending funds and have had a chance to accept just a few less loans:
-
list serves – check list serves, sometimes your line of work already qualifies you enough to at least apply when an opportunity comes up
-
research office and development – they’re really good about aligning you with opportunities that fit both your niche research and your background
-
your PI can be a huge source of leads – a good PI will gladly help you find money to help keep you around, especially if you’re pulling your weight
Again, this isn’t meant to be a definitive guide, I’m just explaining how I personally found a research opportunity and how I decided to handle the negotiations.
If you’re a premed, you might want to read up on the older articles about how to find research as an undergrad:
https://doctororbust.wordpress.com/2014/02/08/research-doing-research/
We Have A Free-ish Weekend!!! Life Updates and Stuff
Hello,
Between the last post, about two weeks ago, and this one we’ve taken two exams: Cardiovascular System and Neurology. There is one exam, for each subject, you either pass them or you fail them.
Passed 🙂
We start a new unit on Monday, so there’s a brief interlude where I have nothing to do! Sort of.
Let me start with what happened right after my cardiovascular exam, that was two weeks ago. The exam was placed on Wednesday. Right after the exam, that Thursday morning, we had a mandatory discussion on Neurology — hours of suggested review and reading was ‘suggested’. Friday, I was scheduled to give the flu shot, followed by Integrated Problems presentation and group work. Fortunately, the flu shot was canceled, unfortunately life thought it’d be funny to make me sick instead. I made it through most of the day, went home and pretty much hacked up my lungs throughout the 3-day weekend of Neurology. I’m pretty sure it wasn’t the flu, but it just went from a simple cold to something rather wicked combined with my asthma. Considered going to urgent care for a nebulizer, if my oxygen saturation dropped more than it had (I was at a do-able 95%, down from my usual near 99-100%). After a few days, the cold was gun, but the congestion was just ridiculous. On top of that, class was still going on (4 lectures a day), as well as my part on the research project, and trying to maintain a healthy relationship.
Everything worked out, I hit my deadlines with the patient and subject (controls) enrollment, didn’t flake on my commitments to friends, and I did well in Neurology. Ok, sure, one patient we couldn’t enroll in the study but wanted to join at one time sent me a “poop” emoji. But, I’m really learning how to let things roll off my back — in fact, I think the “poop” emoji is sort of hilarious, how does one professionally respond to a “poop” emoji as the only text you receive without any previous texts?
After a week, I was feeling well enough to enjoy myself again. I’m learning to better use my time as well, and how to take a break — I even went to a Japanese tea ceremony instead of studying this past Sunday.For me, that’s a big deal, it’s breaking the cycle of ruminating. A friend from college flew in from California on vacation, so I squeezed in sometime after clinical assignments to eat a vegan restaurant. I’m not vegan, she was, but good food is good food.
And now, the exam is over and there’s a lull before the next part of the module begins. My project is coming to a close, it looks like we’ve went from hopeless to actually having the pilot have made enough progress to submit for funding in the coming weeks. I feel like the being busy and pushed into a corner forced me to work on my priorities and better schedule myself, I also hope that it reset my stress ‘thermostat’ to better setting while juggling responsibilities.
The following aren’t so much tips, as they are just a record of how I personally got through a pretty tough patch. The first year, I thought there weren’t enough hours in the day for what they asked us to do. I have a long way to go, but I think I’ve grown a little in terms of time management. From here forward, I will probably use the following system the rest of the year and try to improve them as time goes along:Work with a partner, and divide up the material. This takes a lot of trust, that’s the hardest part of this strategy. Everyone in class is smart, so that’s not a problem. Indeed, it’s likely everyone in a medical school class was that one person who got stuck doing all of the “legitimate” work on group projects as an undergrad. As soon as you find a person you can literally spend all day with for weeks prepose to make that study buddy relationship official.
- My partner and I split the work 50/50, for no particular reason I took the odd lectures and they took the evens. We would make study guides for each lecture, and present the study guide orally (and the logic) every few days in person or on Skype.
- Close to the exam, when we did a full review, we then present the lectures again at a faster rate but this time we’d switch the lectures (I did evens, they did odds).
- Work on practice questions separately, then discuss the questions, stems, and all the answer choices — it was usually a good exercise to figure out why the wrong answers were wrong and modify them to make them right.
- I kept a running list of things I feel I needed to work on, for example if I noticed I sucked at a particularly subject I’d note it then go read more about it. I found checking PubMed and UpToDate was usually very helpful to put things into context for clinical relevancy. In my notes, I found it was very helpful to keep track of my citations when I learn something new.
- When I was most lucid, I’d make a priority to do list every so often to take stock of where I was in the day/week. Sometimes, I’d noticed the most important task for the day was to run through Anki pharmacology cards, sometimes the most important task (time wise) was to phone patients/subjects, at other times I found the most important task was just to assess my situation.
- To keep on top of my research I just tried to keep in close contact with my PI with occasional meetings, we often exchanging text messages, or emails, and the occasional evening calls to touch bases. Keeping a transparent relationship on the project made things very doable.
And now, I’m pleasantly enjoying my night off. Sure, I have stuff to do this weekend: signed up for nurse shadowing this weekend, have to contact some patients/subjects. So, I’m not totally off, but at least I get to take a nice mental break. Next week, I’ll return to the cardiology wards for a few morning rounds with my PI’s cardiology team. The project is coming to a close, and this next module of medical school will be a lot easier on time since I don’t expect to be sick or jump on any emerging pilot projects for any time soon — I hope.
October Updates – MS2 + Research (Again!)
Cardiovascular Exam on Wednesday Yesterday
We’re well into half of the first semester. This block of courses was Pulmonary (finished) and Cardiovascular. Mixed into our ‘classroom’ time we’re also scheduled for didactics training, and interspersed among everything we have workshops on medical imaging (X-rays, CT scans, etc). It’s our last year of ‘classroom’ time, from next year we take the boards and hit the wards and pretend to be doctors — I keep using the parenthesis with “classroom” because I don’t actually go to class unless it’s a discussion, skills training, or seminar. I spend most of my time studying like I did for the MCAT, at a cafe with headphones — I find studying in public really helps to break up the monotony, and it’s nice to strike up a random conversation with a stranger (I’m Californian).
Started Project
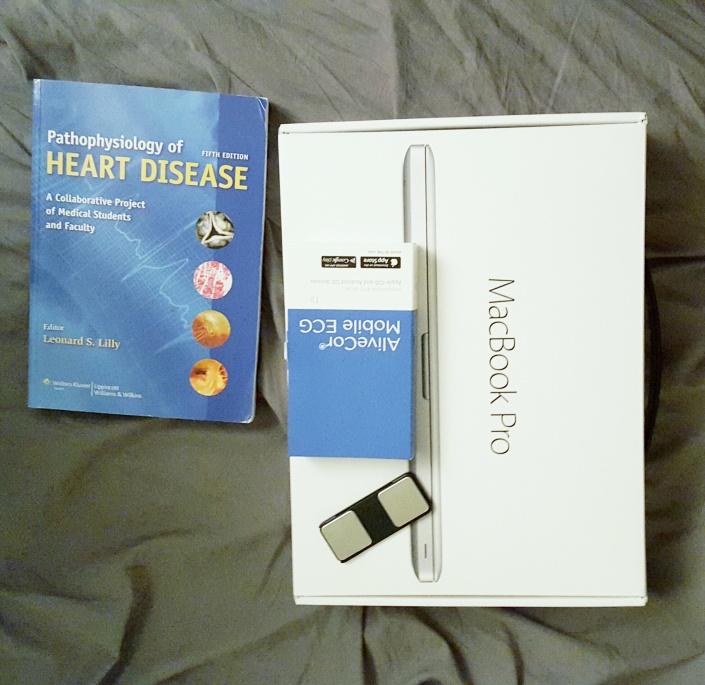
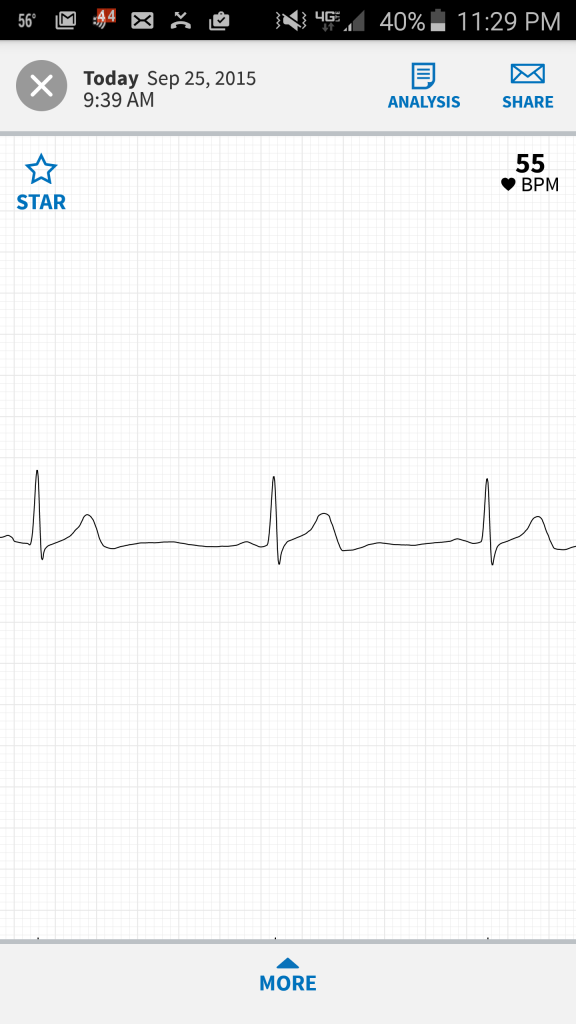
In the summer between MS1 and MS2 I had a project in the cardiology department. In the project I made new friends, and I even gained a role model. With that project completed, and classes ongoing, I received an email asking to help with another project. I like having projects, it keeps me busy and out of trouble — idol hands. Monday, I traveled to pick up the proprietary software/laptop I’ll be using for the project. A week ago I received a batch of portal ECG device I’ll use with patients, and from today I started on recruitment. It’s going to be a tough schedule for the next few weeks, this pilot project should be done in two weeks. The neurology part of this block also has its exam in two weeks. There is free time in medical school, I’ll just have to use it judiciously in the next few weeks. Anyways, I’m really excited I get to help with this project because I believe the results will be generalizable. Selflessly, a large bonus is that I believe this project’s scope will help my own parents health. I want to talk more about it, but half of the project is still proprietary and the hard work didn’t come from me.
I believe it was around this time, two years ago, that I interviewed at my program. Because cardiovascular disease has literally plucked those I care about away, I ended up dropping all interests of PhD programs to become a MD. I have no idea if I’ll be a cardiologist, if I’m qualified to be one, or if I’ll still be interested when it comes time to apply for that fellowship. But, what do do know is that I’m grateful that I even have that as an open possibility.
Best Wishes to Applicants
Hey,
Through the medical education onslaught it’s easy for me to lose appreciation for how it felt to apply to medical school. It’s funny how quickly you lose touch with time and reality. But, right now there’s a new batch of premedical applicants applying. And if you’re one of them this cycle, then my hat’s off to you! Regardless if you received an interview, I congratulate you on just clicking the submit button — there’s a world of a difference between intending to apply to medical school and being committed as an applicant. There’s a whole lot of reasons, but most people never get the opportunity to apply. So, if you are good luck and focus on being well!
I think interviewees start arriving, at our program, in a few weeks. This Monday there’s a free dinner an opportunity to learn how we can help in the admissions process. Last year, I participated in the admissions days, it was fun and I think I’ll do it again. It’ll be fun to see bright, hopeful, and lively faces around the medical campus again. The first time I saw interviewees as a medical student, awkwardly enough, was while I was holding someone’s severed leg — you build lots of hallmark moments in the first year. I was lucky to meet a few more during a less odd social setting. Last year, I even met someone who reads my blog, that was a pretty cool situation. [if you’re reading this thanks for reading, and hope you got in somewhere!]
My Medschool Updates
So, as a second year medical student, we just finished our first block of classes (Pharmacology, Pathology, Infectious Disease and a deluge of Drugs). We had the final exam this morning, it went well, so I’m happy. I used Sketchy Medical School, i.e. Sketchy Micro, for most of the microbe stuff. It was great. Also, I found a pretty decent study schedule/groove. My schedule isn’t so bad this year. I wake up at about 9-9:30 AM, I watch almost all lectures from home at 2x speed. You see, going to school by public transportation rips 1-1.5 hours out of my day. In the time it takes for me to transport myself, I could have already finished watching the day’s lectures. With my current agenda: I then leave my house to study, for about 5 hours a day I study alone or with a friend. I return home, get my fair share of cat videos watched, eat and preview for the next day of studying. I really enjoyed this schedule, because I had a lot of free time and time to get work done, hopefully it’ll work just as well for this coming Pulmonary Disease/Drugs block.
Besides the normal courses, our clinical training starts back up next week. Honestly, I have no idea what this entails in detail. I assume, it’s sort of like a role-playing-game, every time we level up in ability we’re given new challenges we couldn’t have handled before. Most of my time will be spent at a community clinic. Concurrently, I contacted a physician I worked with this summer in cardiology, my plan is to spend some time in both ambulatory and inpatient service cardiology — I really enjoyed the previous experience. Aside from that, not sure if I’ll be accepted, but I just applied to two community service programs with other friends/classmates. I’m really crossing my fingers, I knew about one particular outreach program before I even applied to this school, in fact it was the very reason I found out about this medical school in the first place. If things work out, I’ll update you.
Today, I just gave a mock medical school interview via Skype. It was fun. They sent me their AMCAS application, personal statement, and some secondary applications. My job is to read all of it, and make a mock interview out. Turns out, it’s epically faster to read someone’s applicant rather than to write it, it didn’t take very long to go through their application. I have a much better working memory than when I started school, so that helps. And, now that I know a few people who are on the admissions committee I have an even better understanding of what they’re trying to accomplish during the interview. Personally, I really like interviewing and I find it to be the easiest part, it’s a lot less hum-drum than cranking out application essays — in the past it was rare that I wouldn’t get a job if I scored an interview, and I was accepted at all programs where I interviewed. I consider myself an introvert, that’s a big reason why with my free time I’d rather be drinking coffee [alone] and writing, but I can turn on the interpersonal skills when needed. If you’d like some tips on how to tackle your shyness for the interview feel free to email me.
If you’d like to read more medical school interviews, at least my experience of it, then you can read more right below:
What my medical school interviews were like
Blog Updates
Good luck and enjoy your day!
Thanks for reading